The Visian ICL (Implantable Collamer Lens) is an alternative to LASIK offered at the Silk Vision and Surgical Center that allows for the correction of nearsightedness without the use of a laser. The Visian ICL is an intraocular lens; a clear, implantable lens that is placed behind the iris of the eye.

The Visian ICL is made of a biocompatible collagen material that is soft, clear, and flexible enough to be folded during implantation. It cannot be detected by the naked eye.
How is the Visian ICL different from LASIK eye surgery?
The Visian ICL is an alternative to LASIK that does not involve the use of a laser to correct nearsightedness or myopia. In many cases, those that are not candidates for LASIK are likely to be candidates for the Visian ICL implant. Instead of using a laser to reshape the corneal surface of the eye, a small incision is made in on the far edge of the cornea, and the folded Visian ICL lens is implanted through the incision. The lens gently unfoldsin the eye, and is then its four corners are placed behind the iris.
Am I a candidate for the Visian ICL?
Candidacy for the Visian ICL is generally contingent upon several factors, but the Visian ICL may be a good option for correcting your myopia if:
- You are aged between 21 and 45
- You are nearsighted, with low to high myopia at -3 diopters to -20 diopters.
- You have had stable vision for at least one year
- You have minor (or no) astigmatism
- You have dry eyes
- You have thin corneas, which may render you ineligible for LASIK
What are the benefits of choosing the Visian ICL?
The Visian ICL is a great alternative to LASIK eye surgery; it is an outpatient procedure that typically takes no longer than fifteen minutes and has a low recovery time of only a few days. In some cases, intraocular lenses (such as the Visian ICL) can produce better and more predictable visual outcomes than with laser vision correction.
With the Visian ICL, the corrective lens is selected based on your individual prescription, so you can rest assured that the results are tailored to your visual needs. For more information about the Visian ICL, contact us at Silk Vision and Surgical Center today!
LASEK & PRK
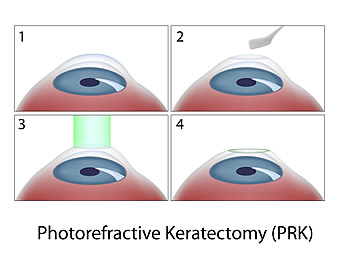
These procedures are similar to LASIK, except that a tissue flap is not created. The laser treatment is done on the surface of the eye after removing the outer layer of cells. LASEK and PRK are suitable for people whose corneas are too thin or too curved to be good candidates for standard LASIK. With LASEK and PRK, healing time is slightly longer than with LASIK, and good vision is achieved in four to seven days.
In general, the conditions we are able to treat include nearsightedness (myopia), farsightedness (hyperopia) and astigmatism. We like our patients to be at least 18 years of age, have healthy corneas, and to have had stable vision over the past year.
What should I expect before, during, and after surgery?
What to expect before, during, and after surgery will vary from patient to patient, the following is a compilation of patient information to inform you about what to expect. Dr. Silk will be able to explain the process in greater detail during your LASIK evaluation.
Before Surgery
If you decide to go ahead with LASIK surgery, you will need an initial or baseline evaluation by your eye doctor to determine if you are a good candidate. This is what you need to know to prepare for the exam and what you should expect.
If you wear contact lenses, it is a good idea to stop wearing them before your baseline evaluation and switch to wearing your glasses full-time. Contact lenses change the shape of your cornea for up to several weeks after you have stopped using them depending on the type of contact lenses you wear. Not leaving your contact lenses out long enough for your cornea to assume its natural shape before surgery can have negative consequences. These consequences include inaccurate measurements and a poor surgical plan, resulting in poor vision after surgery. These measurements, which determine how much corneal tissue to remove, may need to be repeated at least a week after your initial evaluation and before surgery to make sure they have not changed, especially if you wear RGP or hard lenses. If you wear:
- Soft contact lenses, you should stop wearing them for 2 weeks before your initial evaluation.
- Toric soft lenses or rigid gas permeable (RGP) lenses, you should stop wearing them for at least 3 weeks before your initial evaluation.
- Hard lenses, you should stop wearing them for at least 4 weeks before your initial evaluation.
Tell your doctor:
- About your past and present medical and eye conditions
- About all the medications you are taking, including over-the-counter medications and any medications you may be allergic to
Your doctor should perform a thorough eye exam and discuss:
- If you are a good candidate
- What the risks, benefits, and alternatives of the surgery are
- What you should expect before, during, and after surgery
- What your responsibilities will be before, during, and after surgery
You should have the opportunity to ask your doctor questions during this discussion. Give yourself plenty of time to think about the risk/benefit discussion, to review any informational literature provided by your doctor, and to have any additional questions answered by your doctor before deciding to go through with surgery and before signing the informed consent form.
You should not feel pressured by your doctor, family, friends, or anyone else to make a decision about having surgery. Carefully consider the pros and cons.
The day before surgery, you should stop using:
- Creams
- Lotions
- Makeup
- Perfumes
These products as well as debris along the eyelashes may increase the risk of infection during and after surgery. Your doctor may ask you to scrub your eyelashes for a period of time before surgery to get rid of residues and debris along the lashes. Also before surgery, arrange for transportation to and from your surgery and your first follow-up visit. On the day of surgery, your doctor may give you some medicine to make you relax. Because this medicine impairs your ability to drive and because your vision may be blurry, even if you don’t drive make sure someone can bring you home after surgery
During Surgery
The surgery should take less than 30 minutes. You will lie on your back in a reclining chair in an exam room containing the laser system. The laser system includes a large machine with a microscope attached to it and a computer screen.
A numbing drop will be placed in your eye, the area around your eye will be cleaned, and an instrument called a lid speculum will be used to hold your eyelids open.
Your doctor may use a mechanical microkeratome (a blade device) to cut a flap in the cornea. If a mechanical microkeratome is used, a ring will be placed on your eye and very high pressures will be applied to create suction to the cornea. Your vision will dim while the suction ring is on and you may feel the pressure and experience some discomfort during this part of the procedure. The microkeratome, a cutting instrument, is attached to the suction ring. Your doctor will use the blade of the microkeratome to cut a flap in your cornea. Microkeratome blades are meant to be used only once and then thrown out. The microkeratome and the suction ring are then removed.
Your doctor may use a laser, instead of a mechanical microkeratome, to cut a flap on the cornea. If a laser keratome is used, the cornea is flattened with a clear plastic plate. Your vision will dim and you may feel the pressure and experience some discomfort during this part of the procedure. Laser energy is focused inside the cornea tissue, creating thousands of small bubbles of gas and water that expand and connect to separate the tissue underneath the cornea surface, creating a flap. The plate is then removed.
You will be able to see, but you will experience fluctuating degrees of blurred vision during the rest of the procedure. The doctor will then lift the flap and fold it back on its hinge, and dry the exposed tissue.
The laser will be positioned over your eye and you will be asked to stare at a light. This is not the laser used to remove tissue from the cornea. This light is to help you keep your eye fixed on one spot once the laser comes on.
When your eye is in the correct position, your doctor will start the laser. At this point in the surgery, you may become aware of new sounds and smells. The pulse of the laser makes a ticking sound. As the laser removes corneal tissue, some people have reported a smell similar to burning hair. A computer controls the amount of laser energy delivered to your eye. Before the start of surgery, your doctor will have programmed the computer to vaporize a particular amount of tissue based on the measurements taken at your initial evaluation. After the pulses of laser energy vaporize the corneal tissue, the flap is put back into position.
A shield should be placed over your eye at the end of the procedure as protection, since no stitches are used to hold the flap in place. It is important for you to wear this shield to prevent you from rubbing your eye and putting pressure on your eye while you sleep, and to protect your eye from accidentally being hit or poked until the flap has healed.
After Surgery
Immediately after the procedure, your eye may burn, itch, or feel like there is something in it. You may experience some discomfort, or in some cases, mild pain and your doctor may suggest you take a mild pain reliever. Both your eyes may tear or water. Your vision will probably be hazy or blurry. You will instinctively want to rub your eye, but don’t! Rubbing your eye could dislodge the flap, requiring further treatment. In addition, you may experience sensitivity to light, glare, starbursts or haloes around lights, or the whites of your eye may look red or bloodshot. These symptoms should improve considerably within the first few days after surgery. You should plan on taking a few days off from work until these symptoms subside. You should contact your doctor immediately and not wait for your scheduled visit, if you experience severe pain, or if your vision or other symptoms get worse instead of better.
You should see your doctor within the first 24 to 48 hours after surgery and at regular intervals after that for at least the first six months. At the first postoperative visit, your doctor will remove the eye shield, test your vision, and examine your eye. Your doctor may give you one or more types of eye drops to take at home to help prevent infection and/or inflammation. You may also be advised to use artificial tears to help lubricate the eye. Do not resume wearing a contact lens in the operated eye, even if your vision is blurry.
You should wait one to three days following surgery before beginning any non-contact sports, depending on the amount of activity required, how you feel, and your doctor’s instructions.
To help prevent infection, you may need to wait for up to two weeks after surgery or until your doctor advises you otherwise before using lotions, creams, or make-up around the eye. Your doctor may advise you to continue scrubbing your eyelashes for a period of time after surgery. You should also avoid swimming and using hot tubs or whirlpools for 1-2 months.Strenuous contact sports such as boxing, football, karate, etc. should not be attempted for at least four weeks after surgery. It is important to protect your eyes from anything that might get in them and from being hit or bumped.
During the first few months after surgery, your vision may fluctuate.
- It may take up to three to six months for your vision to stabilize after surgery.
- Glare, haloes, difficulty driving at night, and other visual symptoms may also persist during this stabilization period. If further correction or enhancement is necessary, you should wait until your eye measurements are consistent for two consecutive visits at least 3 months apart before re-operation.
- It is important to realize that although distance vision may improve after re-operation, it is unlikely that other visual symptoms such as glare or haloes will improve.
- It is also important to note that no laser company has presented enough evidence for the FDA to make conclusions about the safety or effectiveness of enhancement surgery.
Contact your eye doctor immediately, if you develop any new, unusual or worsening symptoms at any point after surgery. Such symptoms could signal a problem that, if not treated early enough, may lead to a loss of vision.











.png)
