The cornea is the window of the eye. Light travels through the cornea past the lens to the retina and then the brain to form a visual image. The normal corneal surface is smooth and aspheric i.e. round in the center, flattening towards its outer edges. Light rays passing through it moves in an undistorted manner to the retina to project a clear image to the brain.
Keratoconus is a disorder in which the cornea undergoes progressive thinning and is the most common corneal dystrophy in the U.S., affecting one in every 2000 Americans. It is more prevalent in teenagers and adults in their 20s. Keratoconus arises when the middle of the cornea thins and gradually bulges outward, forming a rounded cone shape. This abnormal curvature changes the cornea's refractive power, producing moderate to severe distortion (astigmatism) and blurriness (nearsightedness) of vision. Keratoconus may also cause swelling and a sight-impairing scarring of the tissue.


Studies indicate that keratoconus stems from one of several possible causes:
- An inherited corneal abnormality. About seven percent of those with the condition have a family history of keratoconus.
- An eye injury, i.e., excessive eye rubbing or wearing hard contact lenses for many years.
- Certain eye diseases, such as retinitis pigmentosa, retinopathy of prematurity, and vernal keratoconjunctivitis.
- Systemic diseases, such as Leber congenital amaurosis, Ehlers-Danlos syndrome, Down syndrome, and osteogenesis imperfecta.
Treatment for Keratoconus
Keratoconus usually affects both eyes. At first, people can correct their vision with eyeglasses. But as astigmatism worsens, they must rely on specially fitted contact lenses to reduce the distortion and provide better vision. Although finding a comfortable contact lens can be an extremely frustrating and difficult process, it is crucial because a poorly fitting lens could further damage the cornea and make wearing a contact lens intolerable. In most cases, the cornea will stabilize after a few years without ever causing severe vision problems. But in about 10 to 20 percent of people with keratoconus, the cornea will eventually become too scarred or will not tolerate a contact lens. At this point, surgery may be needed to restore vision. In the past, surgical treatment options were limited and often required long visual recovery time. Now, however, there are new treatment options for patients such as collagen crosslinking with ultraviolet light, INTAC corneal implants, and advanced corneal transplantation techniques such deep anterior lamellar keratoplasty (DALK). These new procedures are less invasive and have faster visual recovery times.
Collagen Cross-Linking
Collagen Cross-Linking
A NEW PERMANENT NON SURGICAL TREATMENT: CORNEAL COLLAGEN CROSSLINKING WITH RIBOFLAVIN®
So far there has been not one successful way to stop the progression of keratoconus. With current methods using rigid contact lens or intracorneal ring segments, only the refractive error (spectacle numbers) can be corrected, but it has very little effect on the progression of keratoconus. It is estimated that eventually, 21% of the keratoconus patients require surgical intervention to restore corneal anatomy and eyesight. A new non-surgical, non-invasive treatment, based on collagen cross-linking with Ultraviolet A (UVA, 365nm) and riboflavin (Vitamin B 2), a photosensitizing agent is now available. This changes the intrinsic biomechanical properties of the cornea, increasing its strength by almost 300%. This increase in corneal strength has shown to arrest the progression of keratoconus in numerous studies all over the world.
What is collagen cross-linking?
A new treatment for keratoconus which has shown great success is Corneal Collagen Crosslinking with Riboflavin, a one-time application of riboflavin eye drops to the eye. The riboflavin, when activated by approximately 30 minutes illumination with UV-A light, augments the collagen cross-links within the stroma and so recovers some of the cornea’s mechanical strength. Developed at the Technische University Dresden, Germany has been shown to slow or arrest the progression of keratoconus, and in some cases even reverse it, particularly when applied in combination with intracorneal ring segments.
Who can benefit from this treatment?
Collagen cross-linking treatment is not a cure for keratoconus, rather, it aims to slow or even halt the progression of the condition. This is important to understand. Patients may need to continue to wear spectacles or contact lenses (although a change in the prescription may be required) following the cross-linking treatment but it is hoped that it could limit further deterioration in the patient’s vision and reduce the case for keratoplasty. The main aim of this treatment is to arrest the progression of keratoconus, and thereby prevent further deterioration in vision and the need for corneal transplantation.
What are the risks and consequences involved?
Very few potential risks associated with this treatment have been reported so far. The Ultraviolet light dose used is designed to prevent damage to the cells that line the back of the cornea or the other structures within the eye. No lens opacities (cataracts) have been attributed to this treatment in European trials. The treatment involves the outer layer (epithelium) of the cornea. There is, therefore, discomfort and a short-term haze. Other lesser but more common risks include:
- Inability to wear contact lenses for several weeks after the treatment
- Changes in corneal shape necessitate fitting of a contact lens or an occasional change in spectacle correction.
As is the case with any treatment, there may also be long-term risks that have not yet been identified. The increased corneal rigidity induced may wear off over time and further periodic treatments may be required.
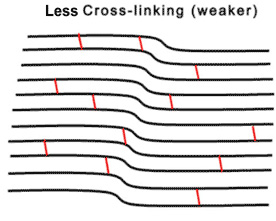
How does Cross-Linking arrest keratoconus?
Until recently, there was no method to change the integrity and strength of the cornea itself for keratoconus patients. The non-invasive treatment of corneal collagen cross-linking riboflavin has been proven to strengthen the weak corneal structure in keratoconus. This method works by increasing collagen cross-linking, which are the natural anchors within the cornea. These anchors are responsible for preventing the cornea from bulging out and becoming steep and irregular (which is the cause of keratoconus).
Are there any published studies for the same?
In published European studies, such treatments are proven safe and effective in patients. The 3 and 5-year results of Dresden clinical study in human eyes have shown arrest of progression of keratoconus in all treated eyes. (Wollensak G. Crosslinking treatment of progressive keratoconus: New Hope. Current Opinion in Ophthalmology 2006; 17: 356 – 360). Biomechanical measurements have shown an impressive increase in corneal rigidity of over 300% after crosslinking. The Dresden, Germany clinical study has shown that in all treated eyes the progression of keratoconus was stopped. In over 53% of those eyes, there was a slight reversal and flattening of the keratoconus by up to 2.87 diopters. Best corrected vision improved by 1.4 lines. This technique has shown great promise in treating early cases of the disease.
Advantages Of Cross-Linking
- Permanent
- Simple- Single- one-hour treatment
- No follow up sittings required
- No need for admission
- Stops the progress and causes regression of disease
- Does not need eye donation as in corneal transplant
- No major precautions
- No injections or stitches
- No incisions as in Intacs or Corneal ring segments
- Quick recovery with short follow up
Intacs
How do Intacs work and how might they help me?
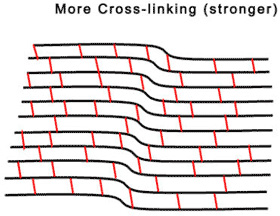
Due to the onset and progression of keratoconus, the weakened cornea loses its natural dome-like shape. As a result, the light rays entering the eye are no longer focused properly, impairing one’s ability to see images clearly.
Intacs are specially designed inserts, made of medical plastic, which are surgically placed under the surface of the cornea. Due to their unique patented design, Intacs are able to remodel the architecture of the cornea re-establishing a more natural dome-like shape and improving one’s vision.
The Intacs Corneal Implant Procedure
Prior to any surgical procedure it is common to experience a degree of anticipation and anxiety. It may be comforting to know that the Intacs procedure is far less invasive than a cornea
l transplant or many other surgical procedures of the eye and the Intacs success rate is high. The surgeons performing the procedure are typically corneal surgeons, having expertise with keratoconus. Each surgeon has also undergone a rigorous training program specific to Intacs for treating patients with keratoconus.
Before the Procedure
Typically, your ophthalmologist, possibly working in tandem with an optometrist will have you undergo a thorough eye examination.
Your examination will include a variety of standard ophthalmic tests for this type of procedure, as well as general medical tests and a review of your specific medical history.
The Intacs Corneal Implant Procedure
Anesthetic drops are used to numb the eye, which is held open throughout the procedure to prevent blinking.
Step 1: A single, small incision is made in the surface of the cornea.
Step 2: The eye is prepared for Intacs placement.
To stabilize your eye and ensure proper alignment of the Intacs inserts, the centering guide is placed on the surface of your eye. During this time, inner layers of the cornea are gently separated in a narrow circular area to allow for Intacs placement.
Step 3: The Intacs inserts are gently placed.
After the second Intacs insert is placed, the small opening in the cornea is closed.
Step 4: The procedure is completed.
The placement of Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision.
Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision.
As with any surgical procedure, there are some risks, including infection. Some patients experience visual symptoms including difficulty with night vision, glare, halos, blurry and fluctuating vision.










.png)
